Actions: Suspected Diphenhydramine Overdose demand attention—now more urgently than ever. The CDC reports that antihistamines were present in 15% of U.S. overdose deaths in 2019–2020, with diphenhydramine responsible for 3.6% of fatalities overall. Overdose outcomes rose 120%+ in adults 55+.
Even more compelling, when taken in massive doses (over ≥1 g), diphenhydramine causes hallucinations, seizures, coma, and death—making early detection and escalation absolutely critical.
⚠️ The Escalating Consequences: These hidden patterns mean diphenhydramine is no longer just an “allergy pill.” Instead, it is a leading co-factor in overdose deaths, with outcomes that escalate to seizures, heart failure, and sudden death.
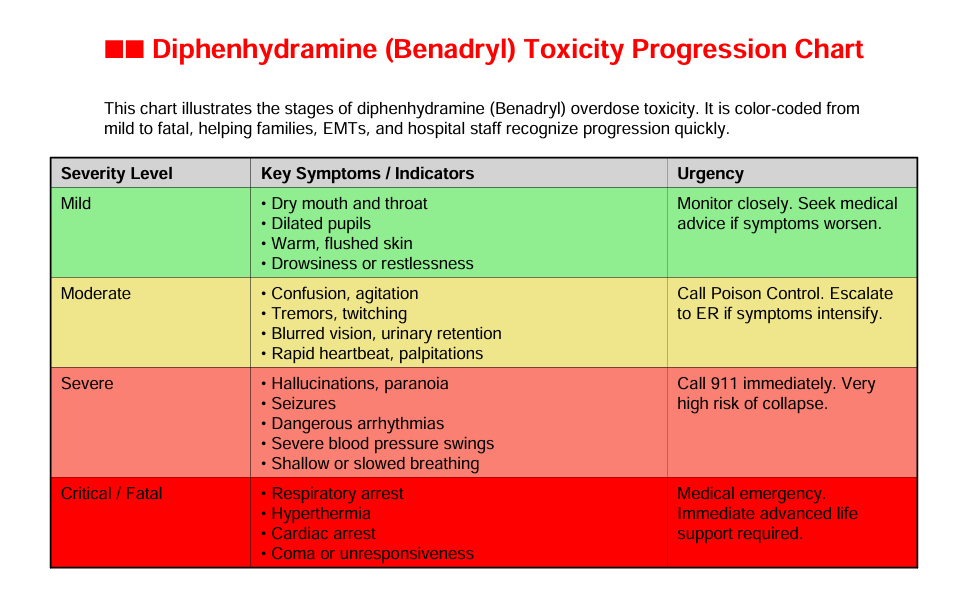
Degrees of Toxicity: From Mild to Fatal
| Severity | Key Signs & Symptoms | Urgency & Action |
|---|---|---|
| Mild | Dry mouth, dilated pupils, warm skin, drowsiness | Monitor, call medical advice if changes appear |
| Moderate | Confusion, agitation, tremors, blurred vision, palpitations | Call Poison Control, escalate to ER as needed |
| Severe | Hallucinations, paranoia, seizures, arrhythmias, low breathing | Call 911 immediately, risk of collapse |
| Critical | Respiratory arrest, hyperthermia, cardiac arrest, coma | Immediate advanced life support required |
Clinicians highlight that serious neurological effects—especially seizures and coma—can emerge at ingestions over 1 g, with risk rising further above 1.5 g. Mortality frequently follows cardiac or respiratory failure if not treated promptly and decisively.
Personal Story—Unintended Toxicity and Fatal Consequence
Background & Progression
John, a 68-year-old retiree, began taking diphenhydramine nightly for allergies and insomnia. However, as sleep continued to evade him, he increased the dose—first doubling, then redosing within hours—unaware that the drug’s delayed onset and slow clearance would cause buildup.
Escalation & Symptoms
Soon after, John showed worsening confusion, frequent falls, and vivid hallucinations. Gradually, his family noticed he was disoriented and unsteady. Nevertheless, they dismissed it as harmless because the medication was over-the-counter.
Crisis & Outcome
One morning, John was found unresponsive. EMS discovered arrhythmia and shallow breathing. Because older adults metabolize diphenhydramine more slowly, cumulative dosing overwhelmed his system. Sadly, John died, with the cause listed as “respiratory and cardiac arrest due to diphenhydramine toxicity.”
Why Older Adults Face Higher Risk
- Delayed clearance increases toxic levels.
- Polypharmacy worsens sedation and fall risk.
- Cognitive decline contributes to unintentional redosing.
- Lack of awareness allows misuse to escalate silently.
According to MedlinePlus and Harvard Health, many older adults use diphenhydramine for sleep despite its strong anticholinergic effects, which heighten risks of confusion, falls, and even fatal overdose
Less-Known Impacts: Everyday Misuse of Diphenhydramine
Why Unintentional Overdose Escalates Easily
Moreover, people often underestimate diphenhydramine’s potency because it’s OTC. Consequently, they may redose for sleep, access large quantities from bulk packaging, or follow harmful social media trends like the “Benadryl Challenge”—which has contributed to hospitalizations and even deaths from seizures and coma.
Call to Action
Therefore, when symptoms escalate—even subtly—act swiftly:
- Observe onset, dose, and symptoms (physical and mental).
- Communicate calmly: “You’re safe. I’m here.”
- Act by calling Poison Control (1-800-222-1222) or 911 for severe warning signs.
- Stay present, reduce stimulation, and offer reassurance to help ground the patient.
Expert Insights
- The FDA warns that excessive diphenhydramine intake can lead to “serious heart problems, seizures, coma, or even death,” urging families to know about the issues surrounding antihistamin misuse and secure medications when risks are identified.
- Utah Poison Control reports that ingestions over 1 g heighten risk of delirium, seizures, and death—and that physostigmine may reverse anticholinergic delirium effectively in many cases—often outperforming benzodiazepines.
Final Thought
Actions: Suspected Diphenhydramine Overdose must guide us from complacency to vigilance. Because diphenhydramine misuse can climb from mild sedation to fatal collapse silently, every moment counts. Prompt recognition, compassionate communication, and rapid escalation can turn a disguised danger into a life rescued.
Degrees of Antihistamine Toxicity
Toxicity develops in stages. Each stage signals the body is struggling, and every progression raises the risk of permanent harm:
- Mild Impact – Early warning signs:
- Dry mouth and throat
- Dilated pupils
- Warm, flushed skin
- Drowsiness or restlessness
- Moderate Impact – Neurological and systemic involvement:
- Confusion and agitation
- Tremors or muscle twitching
- Blurred vision and difficulty urinating
- Rapid heartbeat and palpitations
- Severe Impact – Life-threatening complications:
- Hallucinations and paranoia
- Seizures
- Dangerous arrhythmias (irregular, unstable heartbeats)
- Severe blood pressure swings (hypertension → hypotension)
- Shallow or slowed breathing
- Critical / Fatal Impact – End-stage toxicity:
- Respiratory arrest
- Hyperthermia (dangerously high body temperature)
- Cardiac arrest
- Coma or unresponsiveness
Why the Numbers Matter
Although antihistamines seem “safe” because they are sold over the counter, their misuse is deadly. In fact, the CDC has documented that diphenhydramine and other first-generation antihistamines are the most frequently implicated antihistamines in fatal poisonings. Because misuse often begins with unintentional overdosing—such as mistaking panic attacks for anaphylaxis, redosing for sleep or doubling for allergy relief—patients, families, and providers must educate, observe, and escalate quickly.
Call to Action
When in doubt:
- Stay with the patient. Calm reassurance prevents panic and helps cooperation.
- Observe the signs. Track timing, symptoms, and dose.
- Act immediately. Call 911 for confusion, seizures, irregular heartbeat, or slowed breathing.
- Communicate clearly. Share details with EMS or Poison Control (1-800-222-1222).
Other Actions: Suspected Antihistamine Overdose Resources
- Antihistamine Overdose: Types, Symptoms, and Treatment
- Antihistamines to treat long COVID: What you need to know | Live Science
- Antihistamine Types & Side Effects
- Can Antihistamines Impact Mental Health
- Caution! These Drugs Can Cause Memory Loss
- Common medications linked to subtle shifts in cognitive performance, study finds
- COVID’s Inflammation Linked to Long-Term Brain Effects – Neuroscience News
- COVID LONG-HAUL DAY 1013 – Dawn Christine Simmons
- Hallucinations induced by an antihistamine-decongestant mixture – PMC
- Hidden Effects of Antihistamines on the Brain | Psyclarity Health
- Humanizing Health: Elevate Respect
- Medications and Older Adults | AAAAI
- Long COVID: 12 Most Common Post-Infection Symptoms
- Long COVID’s Cognitive Crisis
- Over-the-counter medications containing diphenhydramine and doxylamine – PMC
- Risks From Common Pain Relivers for Those 50 and Over
- Sleep aids: Could antihistamines help me sleep? – Mayo Clinic
